Emily Ryan's life changed quite literally overnight when she was a freshman in college.
She was studying for final exams and returned from the library at about 10pm. She crept quietly to bed because her roommate was already asleep.
At about 3am, she woke up with intense pain radiating across her back.
READ MORE: Kanye West apologises after repeated anti-Semitic remarks

"I could not feel my legs anymore," Ryan said. She also smelled urine. The sheets underneath her were soaked.
"And as a 19-year-old person, you know, I didn't pee the bed and so it was very surprising."
That terrifying episode launched what would become a 10-year odyssey to find relief from unrelenting pain. Ryan says she finally found it in what some experts think is an unexpected and controversial place — the psychedelic drug ketamine, which she gets through intravenous infusions every 90 days.
READ MORE: How a three-hour car trip saved the lives of hundreds of dogs
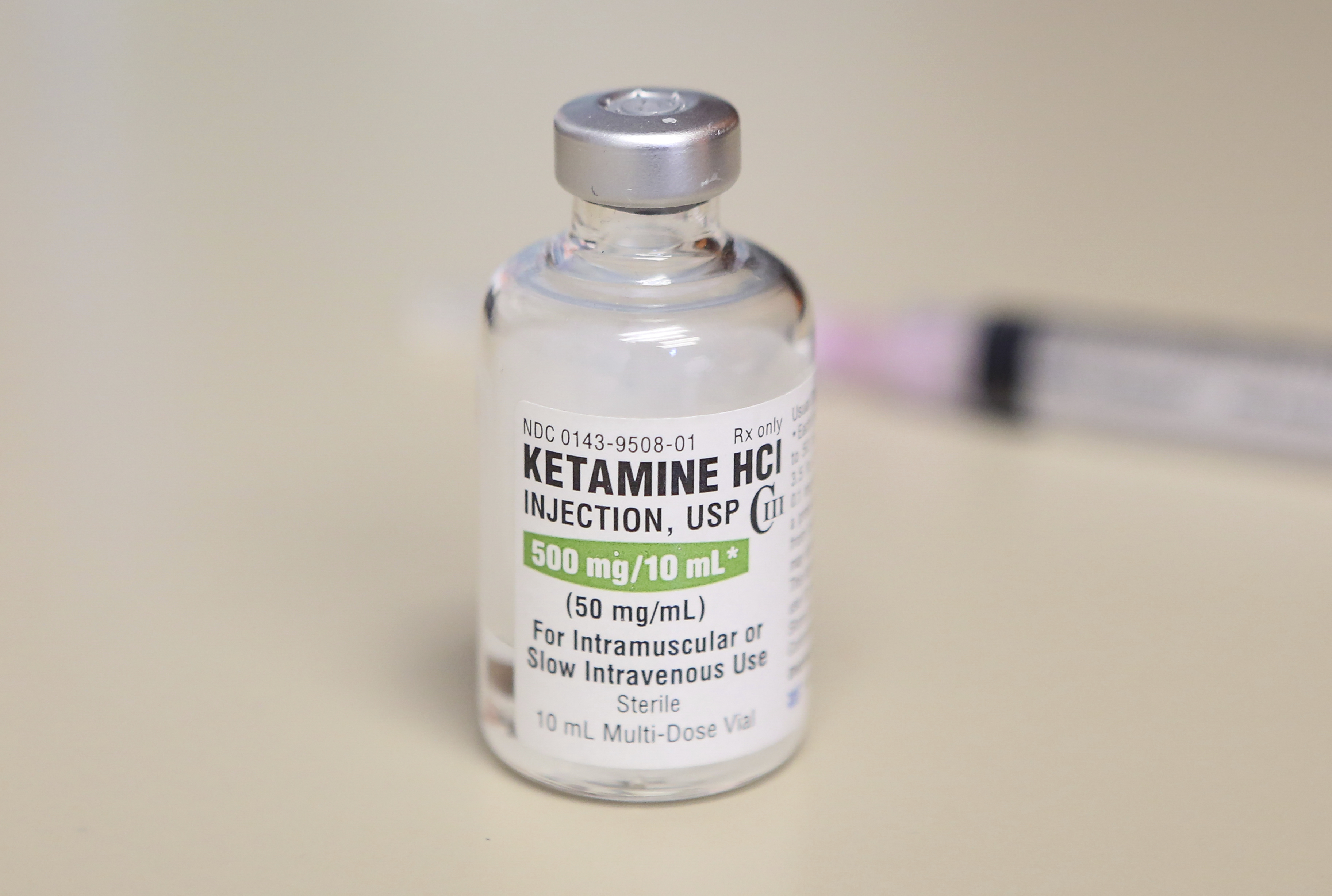
Ketamine has been used as a surgical anaesthetic since the 1970s. It became widely used in field hospitals during the Vietnam War because it doesn't depress breathing and heart rate the way some other kinds of anesthesia can. At the same time, it raises blood pressure and heart rate, which can be helpful for patients who've lost blood.
Like some other psychedelics, ketamine has also proven to be helpful for treating depression and trauma.
A derivative of ketamine — esketamine — was approved by the US Food and Drug Administration in 2019 as a nasal spray for patients with depression that hasn't responded to other treatments.
Some hospitals and specialty pain clinics also use infusions of ketamine off-label to treat intractable pain, like the kind Ryan has.
"A lot of pain docs sort of think it's sort of Voodoo-ish, if you will, sort of like, 'What are you really doing here?'" said Dr Pavan Tankha, a pain specialist at the Cleveland Clinic who is treating Ryan.
Ketamine acts quickly in the body, and it is also cleared quickly, within hours.
Yet Ryan and others who use it for chronic pain say the relief they get after their treatments lasts for months. Experts say it's hard to understand how it could be working for that long, and they point out that while preliminary evidence is promising, there's just not a lot of high-quality research to help explain why it might work or what kind of patient could see the most benefit from it.
Tankha said he was hoping to raise enough money to properly study ketamine's utility for chronic pain.
"The binding to the receptor is over in maybe 10 to 15 minutes, maybe a couple hours, if you're lucky. But why does it work so long?" Tankha said.
"We're studying what I would call the downstream effects from the binding of ketamine. What else is it doing in the brain to cause this lasting relief?" he said.
READ MORE: Restaurateur Bill Granger dies aged 54
A long road to relief
Ryan, who is now 29 and lives in Cincinnati, Ohio, said she did not mind that doctors still had very little understanding of exactly how ketamine helped. She was just grateful that it did, and grateful to have found it.
It was a long road to get to here, though.
When her parents met her at the hospital the night she woke up paralysed in college, doctors initially suspected Ryan might have an infection or kidney stones because there was blood in her urine. They quickly ruled those out.
At the local children's hospital, they put the teen into an MRI machine and gave her a pair of special goggles so she could watch the movie Frozen.
She watched it through once. And then again.
"And on the third time, I thought to myself, 'Something is really wrong if I'm still in this tube.'"
The something turned out to be a tumor pressing on her spine. Fortunately, it wasn't cancer, but the doctors told her it was in a place where it was compressing her nerves. And they admitted that they didn't know how to treat it. Because the tumor was sitting in a risky area, surgery to remove it could paralyse her.
She had to use a walker to get around and lost all control of her bladder. Still, she searched for anything that could relieve her unrelenting pain.
Doctors kept prescribing narcotic painkillers, but both Ryan and her mum said the drugs scared them.
"I don't want to rot my insides and, you know, become addicted to a substance," Ryan said. "That's just very hard if that's going to be the rest of my life."
Surgeons implanted a pacemaker device for her bladder, which has helped with her incontinence. And she became a patient of the pain management program at the Cleveland Clinic.
Ryan tried different procedures, such as epidurals, to try to relieve her pain, as well as longer-term medications. She went to the pain clinic every two weeks for about four years, but nothing seemed to help. In the interim, other tumors have sprung up, also along her spine.
"When I tell you I have tried everything, we have tried everything," Ryan said.
The experience has been financially and emotionally draining.
But Tankha, her pain specialist, wouldn't give up. He suggested Ryan try ketamine infusions, which he said had been used as a treatment for chronic pain since the 1980s.
During his training, Tankha said he was taught that ketamine infusions could be used for a rare condition called complex regional pain syndrome, or CRPS, but that its use should be restricted to that specific diagnosis.
During a stint at the VA hospital in New Haven, Connecticut, Tankha was treating patients with CRPS with ketamine infusions, and another patient — one with a different kind of chronic pain — asked if the same infusions could work for his discomfort.
Tankha explained that ketamine hadn't been studied for the kind of pain he had, but his patient was eager to try, so Tankha agreed.
"We do the infusion, this guy gets four months of relief. And I started scratching my head thinking, 'Well, if it works for him, who else does it work for?'" he said.
How ketamine might disrupt chronic pain
Doctors think that constant pain, such as Ryan's, can rewire the nervous system, making it hypersensitive and easily triggered. This is called centralised pain, or central sensitisation, and it can happen in many different kinds of conditions, including arthritis or fibromyalgia. When this happens, the body starts to make its own pain, in a sense, called neuropathic pain.
"Probably like 15 per cent to maybe 35 per cent of people with arthritis, with neck pain, or back pain, have a very large component of central sensitisation, so they have some arthritis, but their pain is much more severe than their X-rays would would suggest," said Dr Steven Cohen, professor of anesthesiology and critical care medicine at Johns Hopkins School of Medicine.
Cohen helped develop the American Academy of Pain Medicine's 2018 guidelines for the use of ketamine in treating chronic pain.
He says ketamine binds to — and blocks — a receptor in the brain that's responsible for the central sensitisation of pain in the body.
"I hear people say it's like resetting your nervous system," Cohen said.
But that may not fully explain how or why it works. He says in the roughly seven placebo-controlled trials conducted with ketamine for chronic pain, most have been small and patients usually correctly guess when they get it, making it possible that the benefits they reported were a result of bias in the study.
"The evidence isn't super strong," he said.
Cohen said the biological mechanism behind why it might work was also far from clear. If ketamine is blocking key receptors that centralize pain in the body, why would it continue to work long after it's out of a person's system?
Cohen said that ketamine was proven to have lasting impacts on emotion, which was also a big component of the experience of pain; maybe the drug was not acting just on pain signaling in the body but also on the suffering it causes.
"It might be different mechanisms for different people, and maybe there's an overlap," he said.
Over the years, Tankha said he learnt how to refine the treatment. He gives a lower dose of ketamine over a longer period of time to cut down on unpleasant side effects. The infusions last from one to three hours each day in a specialty clinic where patients are monitored and supported while they hallucinate, or trip. Negative side effects of the treatment can include nausea, vomiting, disorientation, confusion, and loss of coordination. Ketamine can also raise blood pressure and heart rate, as well as increase breathing and heart rate.
Ryan says she takes an anti-nausea drug before her treatments, and she's exhausted afterwards. She goes back to a hotel room and crashes afterwards.
Tankha said ketamine infusions were in use at other specialty pain clinics, but they tend to be offered because a specific provider has experience using the therapy. It's not widely available, and clinics that do have it tend to have long waiting lists to get in.
Ryan said she took headphones to listen to music during the session, which lasts between one and three hours. She said she was grateful she's a happy tripper. She said she had visions of her childhood dogs, for example.
"I went in with no expectations because I've tried so many things," Ryan said.
When she got back to her hotel room after the first treatment a little over a year ago, she said she slept for about five hours.
"And I woke up the next day and I was just like, I feel how I did before I got sick," Ryan said.
"I'm completely pain free — 100 per cent pain free," said Ryan, who said she had five or six courses of infusions since then, which were taken over five days at a time.
Ketamine infusions are pricey. Ryan said she was fortunate because the state Medicaid plan she belong to covers her treatments, which have been life-changing. She still has to pay for a hotel room for five days when she travels to get her treatments, and she still has to cover the co-pays. But she thinks it's well worth it.
"I used to take over 40 to 50 pills a day. I'm down to eight a day," said Ryan, who said she still takes the medication gabapentin at night to help with sleep.
But she's now able to work out at the gym, and to spend long hours standing and arranging flowers at the florist business she runs — activities that would have been difficult before. Before the ketamine, Emily says she couldn't walk her dog more than a mile without pain. Now she walks him three or four miles with no issue.
Outside experts caution that every patient may not experience the same good results.
"There are individual people for whom it has been very successful," said Dr. Charles Argoff, who is director of the comprehensive pain center at Albany Medical College.
"But I'm not sure we understand why it's successful long-term for some people and not others. I don't think we completely understand who's likely to benefit from it," Argoff said.
Argoff stressed that it's important to use ketamine under medical supervision with a qualified provider. He said there are ketamine clinics popping up with dubious credentials, and as the actor Matthew Perry's recent death suggests, the use of ketamine without appropriate guardrails may be dangerous.
Insurance coverage for ketamine infusions is also spotty, Argoff said. "So people might be spending lots of money without knowing if it's going to help," he said.
As for Emily Ryan, she said she's back to playing tennis and pickleball and doing the fitness bootcamps she loves.
"Now I go to them with no issues," she said.
